The trainer was Mr. Y.K. Wan and the course scopes included Risk Assessment, Laboratory Practices, Biosafety cabinet, Sterilization and Laboratory Design.
Unacceptable risks can be found during risk assessment. Risk assessment has 5 steps:
Step 1 – gathering information
Step 2 – evaluating risks to health
Step 3 – deciding what needs to be done to control or prevent exposures
Step 4 – recording the assessment
Step 5 – reviewing the assessment
Programs & Committees for laboratory Biosafety are:
- Biosafety Committee
- Biological Agent Inspection
- Workplace Complaints
- Incident Review
- Medical Surveillance
- PPE
- Respiratory Protection
- Equipment Maintenance
- HEPA Filter-containing Equipment Certification
- Safety Training (including Animal Handling, GLP, Spill Control, Signage)
- Emergency Response
- Construction and Renovation
- Facilities Maintenance
- Pest Control
- Waste Control, Treatment and Disposal
Strategic laboratory management of risks on handling biological materials is:
· to develop safety policy and manual
· to implement safety policy
· to determine the risks and the associated Biosafety levels
· to promote safe operational practices in laboratories
· to maintain containment facilities and equipment
· to control import, export, application, and inventory of biohazardous agents
· to provide training to staff and visitor
· to monitor, review, advise the Biosafety management
Biohazardous substances is defined as:
The biological agents such as animals, plants, microorganisms, or the derived substances whatever nature survived or genetically modified that are able to produce deleterious effects on humans, animals, and plants.
Laboratory-acquired infections are transmitted:
- from the agents being directly handled
- by the person who do the laboratory work
- as the result of escape of agents
It may be caused by:
- Inadequate risk assessment
- Inadequate knowledge of disease (e.g. route of infection)
- Improper handling materials (e.g. hidden pathogens)
- Improper handling contaminated equipment and apparatus
- Improper facilities or practices
- Insufficient decontamination
- Insufficient personal protection
One of routes of transmission is Zoonoses which spread between people and animals. Needlestick handling is one of the high risk items. Needle safety should be taken care (Don’t put needle in your lab coat.)

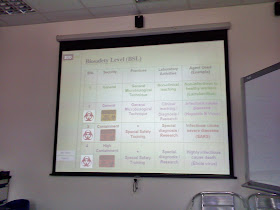
There are four Biosafety Levels (BSL) in the following table.
Biohazard Symbol and label should be used properly.

The Equipment- and technique- related hazards included “Inoculating loop”, “Pipettes”, “Hypodermic needles and syringes”, “Centrifugation”, “Blending, homogenizing and shaking”, “Opening cultures and ampoules”, “Pouring infectious material”, “Breakage and spillage”, “Sharps”, “Ultrasonic devices”, “ELISA equipment”, “Liquid nitrogen”, “Water bath”, “Autoclaves and incinerators”, “Flow cytometer / cell sorter”, “Cryostat microtome”, “Films and smears for microscopy”, “Automated equipment”, etc.
Laboratory Animal should be taken attention!

Laboratory Animal should be taken attention!

Handling biohazardous substances, doubled gloves should be used.
Based on EPD – Practice Notes on the Disposal of Clinical Waste at Landfills, the Solid Clinical / Biological Wastes are classified as follows:
Type 1 – Contaminated Sharps
Type 2 – Laboratory Wastes
Type 3 – Human and Animal Tissue
Type 4 – Infectious Material
Type 5 – Soiled Dressings
Type 6 – Cytotoxic Wastes
Type 7 – Pharmaceutical and Chemical Wastes
Disposal of biological waste should be noticed:
- Register bag packaging system
- Sterilization / Disinfection / Decontamination is required
- Wastes are packaged in leak proof containers
- Sharps must be put into sharp box
- Carcass / organs / tissues are frozen
- Adequate absorbent is placed in package
- Maximum weight of each package are less than 20kg.
Emergency contingency plans has Manual (or SOP / Guidelines) and Training for
- Spillage
- Loss of biological agents (e.g. patient sample)
- Malpractice (e.g. labeling)
- Shutdown of facilities (e.g. exhaust air treatment equipment)
- Security
- Bioterrorism
Different types of Biosafety Cabinet (BSC) were introduced.
The level of sterilant and Disinfectant power are shown.

Lastly, trainer introduced the laboratory design. Risk assessment of building is showed below.

Based on EPD – Practice Notes on the Disposal of Clinical Waste at Landfills, the Solid Clinical / Biological Wastes are classified as follows:
Type 1 – Contaminated Sharps
Type 2 – Laboratory Wastes
Type 3 – Human and Animal Tissue
Type 4 – Infectious Material
Type 5 – Soiled Dressings
Type 6 – Cytotoxic Wastes
Type 7 – Pharmaceutical and Chemical Wastes
Disposal of biological waste should be noticed:
- Register bag packaging system
- Sterilization / Disinfection / Decontamination is required
- Wastes are packaged in leak proof containers
- Sharps must be put into sharp box
- Carcass / organs / tissues are frozen
- Adequate absorbent is placed in package
- Maximum weight of each package are less than 20kg.
Emergency contingency plans has Manual (or SOP / Guidelines) and Training for
- Spillage
- Loss of biological agents (e.g. patient sample)
- Malpractice (e.g. labeling)
- Shutdown of facilities (e.g. exhaust air treatment equipment)
- Security
- Bioterrorism
Different types of Biosafety Cabinet (BSC) were introduced.
The level of sterilant and Disinfectant power are shown.

Lastly, trainer introduced the laboratory design. Risk assessment of building is showed below.

The autoclave is designed with double-door and unidirectional material flow.

The course content was so many and not recorded in details. If you are interested in, please visit HKTIC website at http://www.hktic.org/ to join the next round training.

The course content was so many and not recorded in details. If you are interested in, please visit HKTIC website at http://www.hktic.org/ to join the next round training.
沒有留言:
發佈留言